Thinking about Terminal Care for the Elderly – What it means to attend the deathbeds of the elderly in the age of longevity
Introduction

MASUDA Hiroya, Chairman of Japan Policy Council, Visiting Professor at the University of Tokyo Graduate School
Now that Japan has become a major country of longevity in the world, social security system reform has long been one of the most important national administrative issues. The Council for the Promotion of Social Security System Reform is currently holding a broad range of discussions from a cross-disciplinary perspective with a focus on 2025, when the baby boomers will reach the age of more than 75 years. However, it is the issue of terminal care that is still left behind when medical and nursing care issues are being considered.
Japan’s average life expectancy is the highest in the world, and the percentage of population aging (the ratio of the population aged 65 or over to the entire national population) is over 25%. The number of deaths is also increasing along with this trend, with about 1.2 million people dying in 2014. The number of deaths is projected to reach 1.6 million in 2025, which will mark the arrival of “the age of many deaths.”
One’s home used to be a typical place for Japanese people to attend the deathbeds of the elderly, at a rate of about 70% in 1960. Today, however, about 80% of the elderly die in hospital, and the practice of attending the deathbeds of the elderly at home has long been uncommon. Fewer generations know what it is like to be in the terminal stage, and people have fewer chances to talk about death and attend a deathbed with their family.
The progress of medical technologies has contributed significantly to prolonging life. On the other hand, however, not all terminally ill patients can obtain the desirable medical and nursing care services in terms of quality of life.
The Japan Policy Council held expert study meetings about the way terminal care should be undertaken, and discovered that although intravenous drips and tube feeding for senile and ill elderly people in need of terminal care are common in Japan, this practice is not always common in other countries. In addition, some countries have a system whereby terminal people have prior consultations with doctors to have their wishes reflected in their terminal care and present their documented consensus to medical organizations.
We should not automatically introduce these practices that are carried out abroad to Japan, despite the differences in cultural and cognitive backgrounds. However, this is a challenge that the entire nation should tackle as a country facing an era of the world’s most rapid population aging, and now is the ideal time to start discussing the issue.
We have written this paper in terms of making recommendations about the current situation and future challenges of terminal care for elderly Japanese people from the perspective of medical ethics and home medical care on the basis of surveys undertaken by experts on comparative data with other countries. We sincerely hope that our efforts will be of some assistance for discussions in a range of fields going forward.
June 2015
Masuda Hiroya, Chairman, Japan Policy Council
Introductory chapter: Process of discussions about terminal care in Japan
The progress of medical technologies has made a significant contribution by, for example, making incurable diseases curable. Along with this medical progress, Japan’s average life expectancy has increased, and it currently exceeds 80 years. On the other hand, however, Japanese people have not had sufficient discussions about terminal care for the elderly.
This section outlines the processes of the discussions that have been carried out in Japan to date regarding terminal care and related global trends.
1. Discussion about terminal care in Japan
In the 1970s, the concept of hospices was introduced to Japan, without limiting it to discussions about care for the elderly, and people started to express the need for them. In the 1980s, hospices were actually built and began providing palliative medicine. In response to this situation, the then Ministry of Health and Welfare established the Council for the Examination of Terminal Care in 1987 and started to consider measures for responding to requests from patients and their families by working on problems related to terminal care. In 1990, hospice and palliative care were officially institutionalized as medical insurance application items.
Amid these changes in the social environment, in 1991 we saw the Tokai University Hospital euthanasia case, Japan’s first case in which a doctor was criminally charged with enabling his patient to die easily using drugs. Subsequently, the Kawasaki Kyodo Hospital case of 1998 attracted public attention as the first case in which the Supreme Court announced a judgment on terminal care. The Supreme Court noted that the doctor’s action had been based on a request from the patient’s family; the court dismissed the appeal, claiming that the doctor had not provided appropriate information to the patient’s family and that the patient’s wishes had not been identified. The doctor was convicted of murder.
In 2006, it was revealed that two doctors, who were surgical division chiefs of the Toyama Prefectural Imizu Municipal Hospital, removed artificial respirators from seven patients, including terminal cancer patients, which resulted in their deaths. In 2009, the Toyama District Prosecutors’ Office announced, “The doctors’ series of actions from the introduction of artificial respirators to the removal of artificial respirators were part of their life-prolonging measures and the termination of them, and it is difficult to convict the doctors of murder” and “Even if the doctors had not removed the artificial respirators, the patient might have died at the same time.” The prosecutors’ office dropped the case.
2. Formulate the guidelines on terminal care
The Imizu Municipal Hospital case attracted public attention as a social issue, which prompted the Ministry of Health, Labour and Welfare to formulate the Guidelines on the Decision-Making Process for Terminal Care as the nation’s first policy on terminal care in 2007. In accordance with the direction shown by the court, these guidelines specified how terminal care should be carried out and its procedures, such as respect for the patient’s self-determination right and team-based determination regarding the treatment policy. However, the guidelines did not specify the definition of the terminal stage and the criteria for not subjecting a doctor to criminal charges for terminating life-prolonging treatment.
The Guidelines on Terminal Care formulated by the Japan Medical Association in 2008 did not provide a clear definition of terminal care, saying that it varied from case to case. With regard to indemnification for doctors, the guidelines state, “It is necessary to build a structure for securing the exemption of doctors from civil and criminal responsibility for actions taken in line with these guidelines.” There have been no major cases related to terminal care since the announcement of these guidelines.
For the discussion about the so-called death-with-dignity bills, the Legislators’ Association for Discussing the Legalization of Death with Dignity was established in 2005. Two bills drawn up by the legislators’ association include “respect for self-determination right” and “the doctor’s exemption from responsibility.” The first bill regarded “not starting life-prolonging measures” as an applicable item in the doctor’s exemption from responsibility, and the second bill regarded “terminating life-prolonging measures” as an applicable item in the doctor’s exemption from
responsibility. Both bills dictate that if a terminal patient aged 15 or older shows a documented manifestation of not wishing to receive life-prolonging measures, the doctor should be exempted from legal responsibility for obeying the patient’s wishes. In addition, the bills defined the terminal stage as a situation in which more than one doctor diagnoses the patient as having no chance of recovery even with the appropriate medical treatment when death is imminent. These bills are now being considered, and have yet to be submitted to the Diet.
In around the 2000s, the gastrostomy became common in Japan with a rapidity not seen anywhere else in the world. Currently, many elderly people are fed via a gastrostomy in Japan, and they often suffer from the complication of dementia. Few people can have a gastrostomy removed because of the improvement in their physical condition once a gastrostomy is introduced. However, there are frequent cases where the patient’s family naively agrees to take the doctor’s advice to introduce a gastrostomy, which results in the patient being left bedridden in hospital for many years. It is necessary to give significant consideration to whether such treatment is good for the patient.
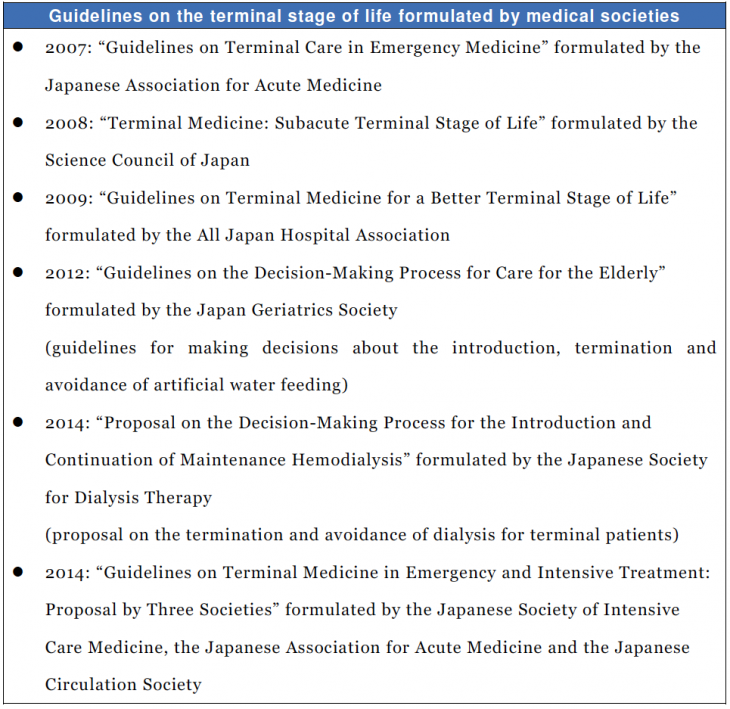
In response to this situation, as shown on the next page (the last page), academia presented guidelines on the terminal stage after the late 2000s.
3. Global trends
As noted in Chapter 4, in European countries, the United States and Australia, it is common to leave terminal elderly people to eat and drink as they like and attend their deathbeds without intravenous drips or tube feeding even after they can no longer eat much. In particular, the government draws up guidelines on palliative medicine in nursing care for the elderly in Australia.
In this connection, some people in Western countries are convinced that excessive life-prolonging medicine should be avoided, particularly for the elderly, and these people have more rapidly embraced a new type of ethics whereby it is desirable for patients to die in peace. The Karen Quinlan case in the United States in the 1970s was a milestone example that led to the endorsement of the avoidance and termination of excessive life-prolonging medicine. This case resulted in the world’s first example of the legalization of the Natural Death Act in California. Today, most states in America have authorized the legalization of death with dignity (natural death) based on a living will (the expression of patients’ wishes in life) as “patients’ human rights.” The living will is also legalized in the United Kingdom, Germany and France.
Translated from “Koreisha no Shumatsuki-iryo wo Kangaeru – Choju-jidai no Mitori (Thinking about Terminal Care for the Elderly – What it means to attend the deathbeds of the elderly in the age of longevity),” “Koreisha no Shumatsuki-iryo wo Kangaeru” (booklet), June 2015, p. 1-7. (Courtesy of Japan Productivity Center) [June 2015]